Heart Health Vitalizer
Scientifically proven to help increase energy at the cellular level while actually boosting the cholesterol-fighting effects of your medication...
Key Ingredients

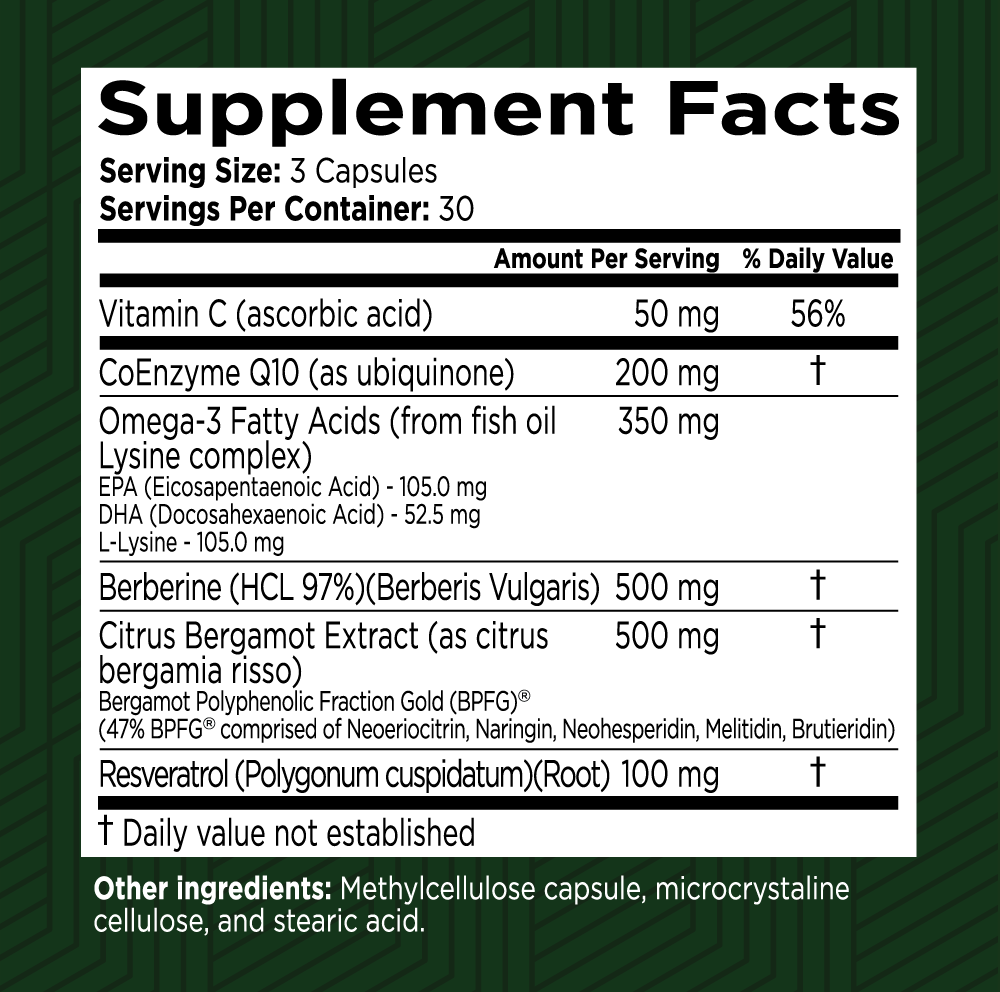
Vitamin C (as Ascorbic Acid)
Vitamin C (as Ascorbic Acid) is a crucial nutrient with a wide range of health benefits. It acts as a powerful antioxidant, supports the immune system, aids in collagen production, and enhances iron absorption. Regular intake of Vitamin C helps protect against oxidative stress, supports cardiovascular and heart health by helping maintain healthy blood vessels and blood pressure, and contributes to the maintenance of healthy skin, bones, and connective tissues. Its role in preventing and reducing the severity of various health conditions makes it an essential component of a balanced, heart-smart diet.

Coenzyme Q 10
Vital to human life, Coenzyme Q10 (CoQ10) plays an important role in cellular respiration, which generates 95 percent of the energy used by the body to support life.

Omega-3 Fatty Acids (from fish oil Lysine complex)
This unique Omega-3 Lysine complex combines essential fatty acids EPA and DHA from fish oil with L-Lysine to support heart, brain, joint, and immune health. Together, they promote healthy inflammation response, cardiovascular function, and tissue repair for whole-body wellness.

Eicosapentaenoic Acid (EPA) as EE
Eicosapentaenoic Acid (EPA as EE) is a powerful omega-3 fatty acid ester that offers numerous benefits for brain health. Extracted from fish oil, EPA is essential for maintaining cognitive function and overall brain health. Here’s a detailed description of its benefits and functions.

Docosahexaenoic Acid (DHA) as EE
Docosahexaenoic Acid (DHA) in its Ethyl Ester (EE) form, stabilized with a Lysine complex, is a premium omega-3 fatty acid ester extracted from fish oil that supports both brain and cardiovascular health. DHA (EE+Lysine) helps maintain healthy cholesterol and triglyceride levels, soothes inflammation in neural and vascular tissue, promotes optimal blood flow, enhances cognitive clarity, and protects both neuronal and endothelial function.

L-Lysine
L-Lysine is an essential amino acid that supports immune function, promotes collagen production for healthy skin and tissue repair, and helps maintain balanced nitrogen levels in the body. It also plays a role in calcium absorption and supports the body’s natural defenses against stress and infection. L-Lysine Complex in our fish-oil formula is chemically bound to EPA/DHA ethyl esters, forming a water-soluble salt that protects these omega-3s from stomach acid and digestive enzymes. This enhanced stability and absorption ensures

Berberine (HCL 97%) (Berberis Vulgaris)
Berberine (HCL 97%) from Berberis vulgaris is a powerful plant alkaloid that supports healthy blood sugar metabolism, lipid balance, and gut health. Clinically studied for its ability to enhance insulin sensitivity and cardiovascular function, berberine offers broad metabolic and anti-inflammatory benefits.

Citrus Bergamot Extract (as citrus bergamia risso)
Bergamot Polyphenolic Fraction Gold (BPFG)®
(47% BPFG® comprised of Neoeriocitrin, Naringin, Neohesperidin, Melitidin Brutieridin)
Citrus Bergamot Extract (as Citrus bergamia Risso) featuring Bergamot Polyphenolic Fraction Gold (BPFG®) provides powerful antioxidant and cardiometabolic support. Standardized to 47% BPFG®—including key polyphenols like Neoeriocitrin, Naringin, Neohesperidin, Melitidin, and Brutieridin—this extract helps support increases in HDL (“good”) cholesterol, aids in reducing LDL (“bad”) and total cholesterol levels, supports balanced blood sugar, and combats oxidative stress.

Resveratrol 99%
This natural polyphenol found in grapes and berries is noted for its antioxidant properties and arterial‐flexibility support. Resveratrol 99% helps replenish the vascular protection lost when cholesterol drug therapy depletes Co-Q10 and other nutrients, and is also being studied for its potential to protect brain cells and prevent age-related cognitive decline.
Frequently Asked Questions
Your health is our top priority
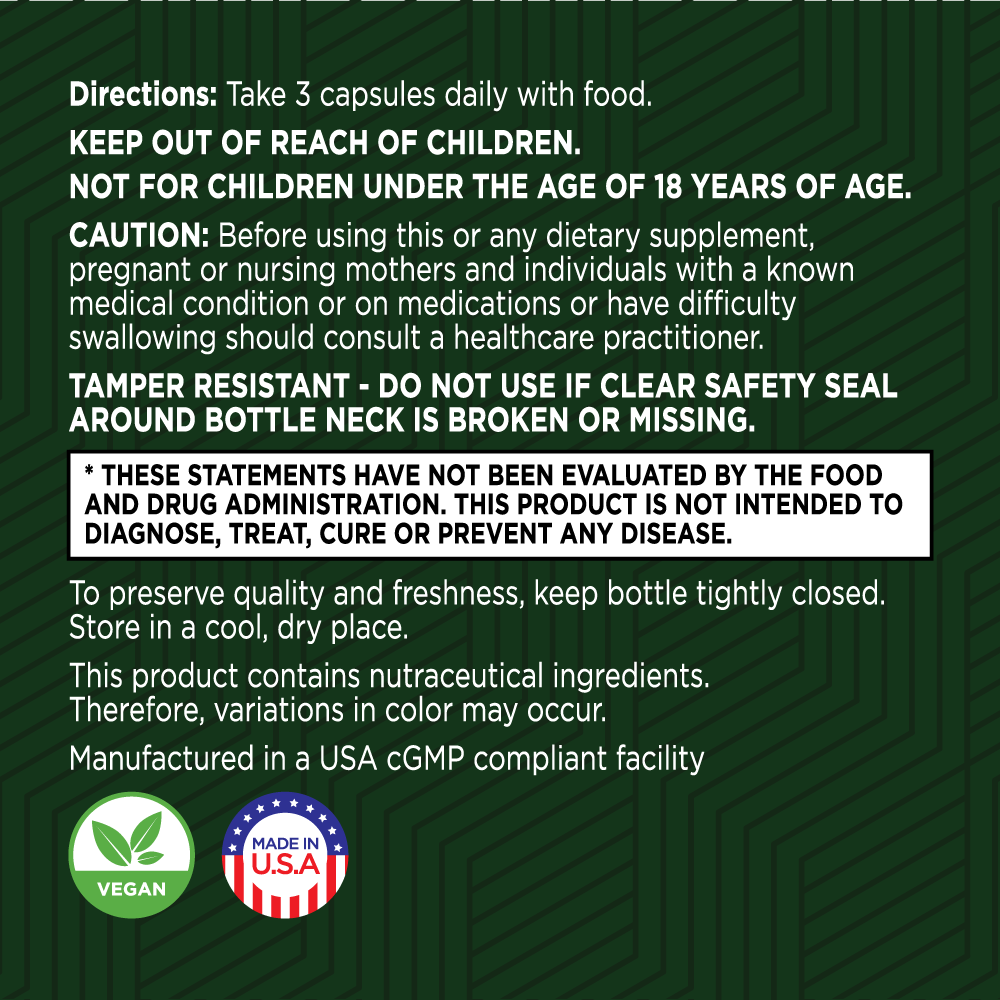
Here at Green Valley, we only work with US-based manufacturing facilities that are cGMP (Good Manufacturing Practices) compliant and FDA inspected.
Our products are triple tested by our manufacturers to ensure potency and purity and are stored in our temperature and humidity-controlled warehouse right here in the Shenandoah Valley, Virginia. And we ship directly to your doorstep – we don’t share warehouse space and we don’t hand off your business to a third party to fulfill your order.
Best of all, all Green Valley products come with our 90-day Satisfaction Guarantee. If you are unhappy with the product for any reason, simply call or email our customer support team and return the unused portion of the product within 90 days of your order. We’ll refund every penny of your purchase (less shipping), no questions asked!