Stem Cell Restore
Increased Energy from Organic Tibetan Sea Buckthorn Trans-Resveratrol, Vitamin D...
Medically reviewed by Dr. Sasson E. Moulavi
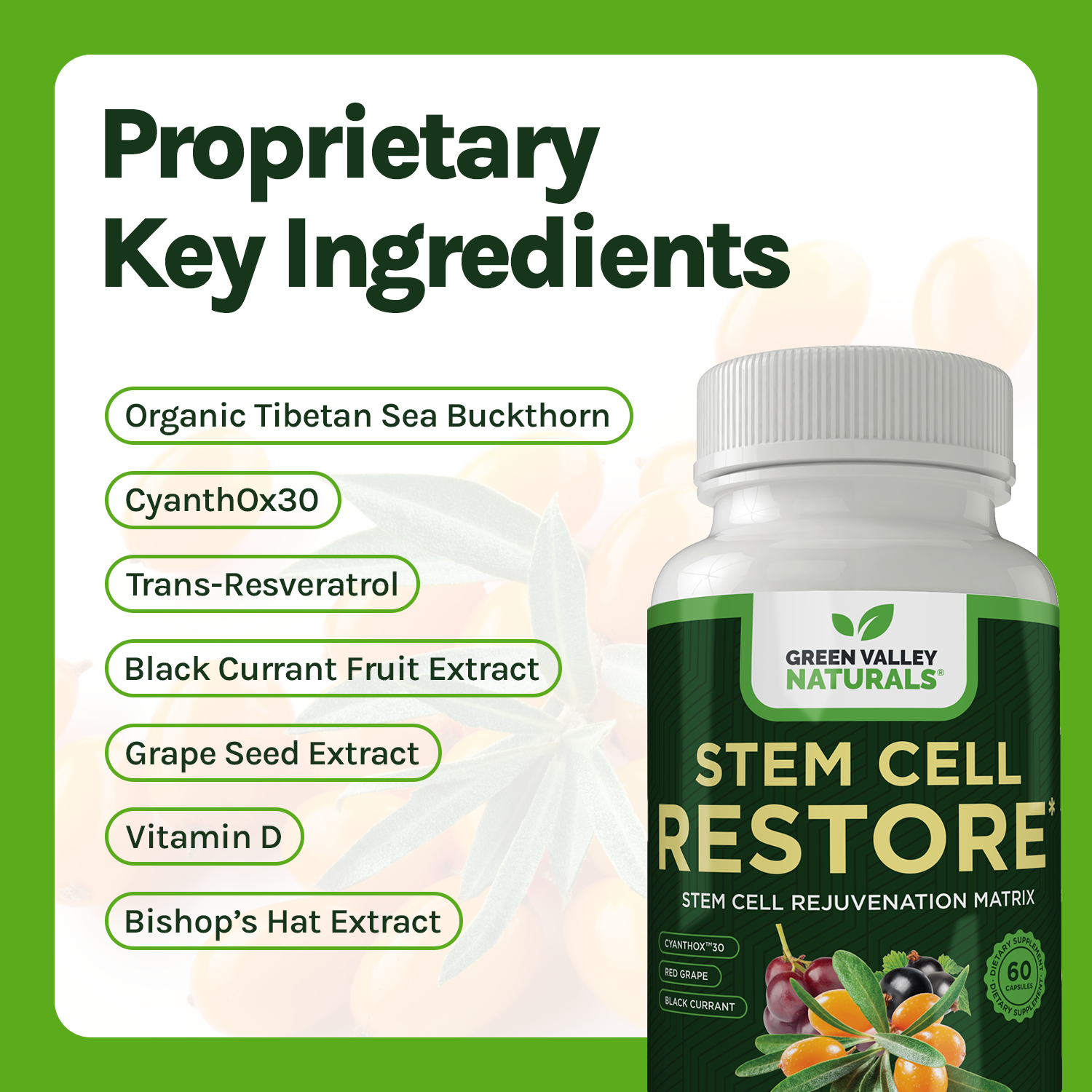
Key Ingredients

Trans-resveratrol (Standardized to 50% (Polygonum Cuspidatum root)
Trans-Resveratrol, a potent polyphenol derived from the root of Polygonum Cuspidatum (Japanese Knotweed), is standardized to 50% purity, ensuring a high concentration of active compounds. Renowned for its significant health benefits, this naturally occurring antioxidant is celebrated for its role in promoting cellular health, longevity, and overall wellness.

Black Currant Fruit Extract (Standardized to 25% Anthocyanins) (Ribes nigrum L. berries)
The combination of Black Currant Extract and Vitamin D3 is utilized for bone health. Black currants have high concentrations of anthocyanins and vitamin C, and when combined with vitamin D3, they help rejuvenate aging bone and bone marrow cells.

Grape Seed Extract (Vitis vinifera seed) (Standardized to 95% Proanthocyanidins)
Rich in oligomeric proanthocyanidins (OPCs), grape seed extract is used for its antioxidant properties and its ability to increase bone marrow stem cell production. It also supports cardiovascular health and brain function.

CyanthOx™M 30 (Organic Tibetan Sea Buckthorn Extract 100:1) (Standardized to 25-35% Proanthocyanidins/OPGs)
Derived from Sea Buckthorn Berry, this extract is highlighted for its potential in boosting stem cells. It's reported to increase several types of stem cells significantly within hours. Additionally, it's rich in antioxidants, with a high ORAC score, indicating a strong potential for enhancing health and longevity.
Vitamin D (as cholecalciferol) (1000 IU)
Vitamin D, provided as cholecalciferol (Vitamin D3), is an essential nutrient that plays a critical role in maintaining overall health. Each serving delivers 1000 IU of Vitamin D3, ensuring an adequate supply to support bone health, immune function, and various other physiological processes. Recognized for its numerous health benefits, Vitamin D3 is vital for maintaining a robust and healthy body.

Bishop's Hat Extract (Standardized to 50% icarin) (Epimedium sagittatum leaf)
Bishop's Hat Extract, derived from the leaves of Epimedium sagittatum, is standardized to contain 50% icariin, ensuring a concentrated and potent dose of this bioactive compound. Known for its remarkable health benefits, this extract is widely recognized for its ability to support bone health, enhance cardiovascular function, and promote overall vitality. Each serving provides a highly effective dose of this traditional herbal remedy.
Frequently Asked Questions
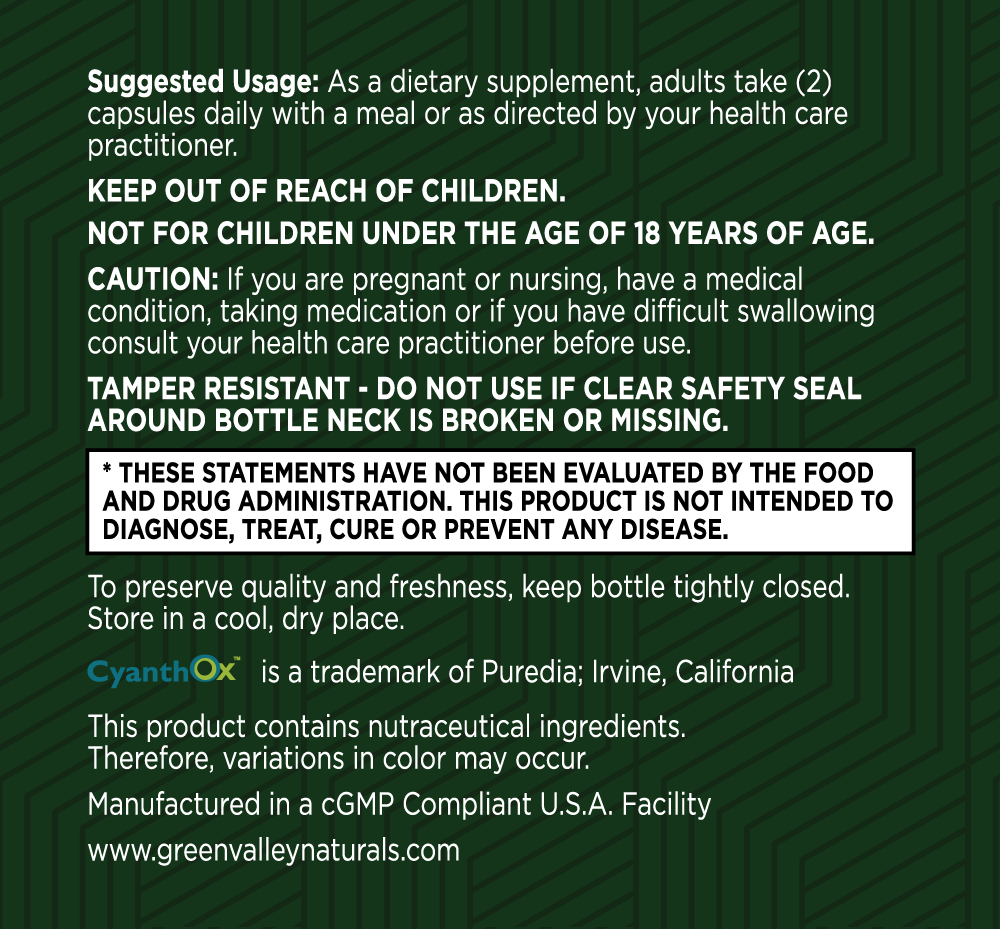
Your health is our top priority
Here at Green Valley, we only work with US-based manufacturing facilities that are cGMP (Good Manufacturing Practices) compliant and FDA inspected.
Our products are triple tested by our manufacturers to ensure potency and purity and are stored in our temperature and humidity-controlled warehouse right here in the Shenandoah Valley, Virginia. And we ship directly to your doorstep – we don’t share warehouse space and we don’t hand off your business to a third party to fulfill your order.
Best of all, all Green Valley products come with our 90-day Satisfaction Guarantee. If you are unhappy with the product for any reason, simply call or email our customer support team and return the unused portion of the product within 90 days of your order. We’ll refund every penny of your purchase (less shipping), no questions asked!

Stem Cell Restore Customer Reviews
After almost 2 months, I feel healthier than before
After almost 2 months, I feel healthier than before. More energy and feel great/younger.
Today is day 56
Today is day 56. I feel stronger and more alert, sleep better, exercise more. I do want to go outdoors and engage in more activities. I feel Much better!
This stem cell is wonderful stuff
This stem cell is wonderful stuff. I just feel so much better and feel more alive inside. There is no comparison. This is the only product that has ever worked for me. With-in the first month I started noticing little small things. I have recommended it to many of my family and friends.
Scientific References
Drapeau, Benson and Jensen, Clinical Interventions in Aging, 2019
https://pmc.ncbi.nlm.nih.gov/articles/PMC9279777/
Priya S, et al. Ad Biomed Pharma. 2017. 4 (1): 1-5.
Bickford PC, et al. Stem Cells Dev. 2006 Feb;15(1):118-23
Ye C, Zhang W, et al. International Journal of Molecular Sciences. 2016;17(11):1780.
Huang, Zhongdi et al. BMC Complementary Medicine 15 (2015):378
CyanthOx Product Brochure
https://www.livescience.com/benefits-of-antioxidants
https://www.nature.com/articles/d41586-024-03936-8
https://www.nature.com/articles/d41586-024-03936-8#ref-CR1
https://www.dvcstem.com/post/stem-cell-supplements
David G Le Couteur, MD, PhD, Rozalyn M Anderson, PhD, Anne B Newman, MD, MPH, Rafael de Cabo, PhD, Stem Cell Transplantation for Frailty, The Journals of Gerontology: Series A, Volume 72, Issue 11, November 2017, Pages 1503–1504
https://en.wikipedia.org/wiki/Proanthocyanidin
CyanthOx Product Brochure (duplicate)
https://pmc.ncbi.nlm.nih.gov/articles/PMC3614633/
Mackie AR, Losordo DW. CD34-positive stem cells: in the treatment of heart and vascular disease in human beings. Tex Heart Inst J. 2011;38(5):474-485
Hajjar I, et al. Circulating Progenitor Cells is Linked to Cognitive Decline in Healthy Adults. Am J Med Sci. 2016;351(2):147-152
Nation DA, et al. Circulating Progenitor Cells Correlate with Memory, Posterior Cortical Thickness, and Hippocampal Perfusion. J Alzheimers Dis. 2018;61(1):91-101
https://pubmed.ncbi.nlm.nih.gov/22146373/
Jin, M., Shi, S., Zhang, Y. et al. Mol Cell Biochem (2010) 344.
Huang, Zhongdi et al. BMC Complementary Medicine 15 (2015):378
Ye C, Zhang W, et al. International Journal of Molecular Sciences. 2016;17(11):1780.
Priya S, et al. Ad Biomed Pharma. 2017. 4 (1): 1-5.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4237620/
Tomé-Carneiro J, et al. Mol Nutr Food Res 2012; 56:810-21.
Brasnyó P, et al. Br J Nutr 2011; 106: 383-9.
Ungvari Z, et al. Am J Physiol Heart Circ Physiol. 2010 Jul; 299(1).
https://pmc.ncbi.nlm.nih.gov/articles/PMC6608268/
https://www.nature.com/articles/srep08075
https://pubmed.ncbi.nlm.nih.gov/16522169/
Bickford PC, et al. Stem Cells Dev. 2006 Feb;15(1):118-23