
Sense of Smell and Longevity: The Surprising Connection Science Reveals
When was the last time you thought about your sense of smell? Most of us take this ability for granted until we lose it temporarily during a cold or sinus infection. But emerging research reveals something remarkable: your sense of smell isn’t just about enjoying the fragrance of fresh coffee or detecting spoiled food—it’s a powerful biomarker for longevity and overall health that may predict your risk of serious disease years before other symptoms appear.
Key Takeaways
· Big health signal, not small symptom: Olfactory decline correlates with 139 conditions and predicts your overall health from your memory to your heart.
· Inflammation is the reason: Elevated inflammatory pathways likely connect smell loss with poor health.
· Practical help is available: Regular, pleasant scent exposure (“olfactory enrichment”) shows promise for memory and inflammation support.
What Your Nose Knows: The Health Risks Hiding in Smell Loss
Scientists studying the connection between sense of smell and longevity have uncovered findings that change how we should think about this often-overlooked sense. Data from large population studies, including the National Social Life, Health and Aging Project, show that olfactory dysfunction (impaired ability to smell) is a higher risk factor for early death than most chronic diseases. In fact, people who score poorly on simple smell tests face significantly higher risks of death within the following decade, even after accounting for age, gender, and existing health conditions.
Even more striking, researchers at the University of California, Irvine and the University of Oxford recently identified 139 diverse medical conditions linked to smell loss—ranging from memory loss and heart issues to nerve dysfunction and poor mood.
The common thread connecting these seemingly unrelated conditions? Inflammation. The loss of smell may serve as an early warning sign that inflammatory processes are affecting your brain and body before other symptoms become obvious.
Understanding this relationship between your sense of smell and longevity could literally add years to your life. Here’s what the science reveals and what you can do to protect this vital sensory system.
Why Your Sense of Smell Declines—And Why It Matters To Your Health
The olfactory system operates through a remarkably direct pathway: odor molecules enter your nasal passages, bind to sensory neurons in the olfactory epithelium (specialized tissue high in your nose), and send signals through the olfactory bulb directly into your brain. Unlike other senses, smell bypasses several intermediate processing steps, connecting straight to brain regions involved in memory, emotion, and cognition.
That's right, the olfactory system is far more than just a gateway to the world of scents—it’s a critical player in brain health. This direct brain connection explains why smell loss often appears early in people suffering problems with their memory or nervous system. The olfactory neurons and their pathways are among the first areas affected by the protein accumulations and inflammatory changes that characterize conditions that affect the brain and cause memory loss. In many cases, people lose their sense of smell years before experiencing memory problems or movement difficulties—making olfactory testing a potential early detection tool.
Brain Health and the Olfactory Bulb: The Overlooked Link
The olfactory nerve is the only cranial nerve directly exposed to the environment, making it especially vulnerable to damage from pollutants, toxins, and infections. This direct exposure means that the olfactory system is often the first to show signs of trouble, serving as an early warning system for broader health issues.
Olfactory impairment has been closely linked to neurodegenerative problems. In many cases, smell loss appears years before cognitive deficits or memory loss, making olfactory testing a valuable tool for early detection. Studies from the National Social Life, Health and Aging Project—a nationally representative sample of older Americans—have shown that olfactory dysfunction is a strong predictor of five-year mortality, independent of other health factors. This makes smell tests a powerful, non-invasive way to identify individuals at high risk for neurodegenerative diseases and other chronic conditions.
The impact of olfactory loss extends beyond physical health. Women’s health research has highlighted that olfactory dysfunction is associated with higher rates of depression, anxiety, and other mental health challenges, which are more prevalent in women. Support from organizations like the McHugh Otolaryngology Research Fund and the American Geriatrics Society has advanced our understanding of how olfactory health intersects with mental well-being and quality of life.
From a clinical perspective, the utility of olfactory testing is gaining recognition. Simple odor identification tests can help predict mortality and flag individuals at high risk for cognitive decline, offering a practical approach for early intervention. Research teams led by associate professors specializing in genetics and the treatment of olfactory and sinus disease emphasize that olfactory dysfunction may be a key mechanism affecting human longevity, and that addressing it could have far-reaching benefits for aging populations.
Is Loss of Smell With Age "Normal?"
Age-related smell loss affects nearly a quarter of people in their early 50s, rising to over half of those over age 80. This isn’t just normal aging that we should accept and ignore.
In clinical assessments, individuals with a normal sense of smell (referred to as 'normosmic') are distinguished from those with impaired or absent smell, which is important for evaluating olfactory function and overall health. The decline reflects cumulative damage to sensory neurons from inflammation, oxidative stress, environmental toxins, infections, and reduced regenerative capacity of the stem cells that normally replace damaged olfactory neurons.
Women generally maintain better smell ability than men, though both genders show progressive decline.
The key insight: smell loss isn’t an isolated problem—it’s a window into systemic health issues affecting your brain and body.
The Longevity Connection: What the Numbers Really Show
The relationship between sense of smell and longevity emerged dramatically from large-scale population studies. One landmark analysis from the National Social Life, Health and Aging Project followed older adults for years after administering simple smell identification tests. The results were sobering:
People with a weak sense of smell had significantly higher mortality risk compared to those with normal smell function—a relationship that remained strong even after controlling for demographics, lifestyle factors, and existing health problems. Olfactory dysfunction is now recognized as one of the strongest predictors of five-year mortality, surpassing many traditional health markers.
But here’s what makes these findings particularly important: smell loss isn’t just a symptom or side effect of disease—it may reflect a causal mechanism. The inflammation that impairs olfactory function appears to be the same inflammatory process driving many age-related diseases.
The Inflammation Connection: Why 139 Conditions Share This Common Thread
When researchers compiled their list of 139 medical conditions associated with smell loss, they initially wondered whether such a diverse collection could possibly share any meaningful connection. The answer turned out to be remarkably consistent: every single condition linked to olfactory dysfunction is also characterized by increased inflammation.
This finding suggests a fascinating possibility—that chronic inflammation doesn’t just accompany smell loss, it may actually cause it. The olfactory epithelium, directly exposed to the environment through your nasal passages, becomes a vulnerable target for inflammatory damage. As inflammation impairs these sensory neurons, smell ability declines. The same inflammatory processes simultaneously affect other organs and systems, setting the stage for conditions ranging from heart problems to memory loss.
Think of smell loss as an early-warning smoke detector for inflammation. Because the olfactory system connects directly to the brain and reflects overall inflammatory burden, changes in smell ability may signal problems years before conventional diagnostic tests detect disease.
This inflammatory connection also explains the wide-ranging consequences of smell loss itself:
Nutritional impact: Food tastes bland without smell, leading to reduced appetite, poor nutrition, unintentional weight loss, and increased frailty. People with smell loss face higher risks of malnutrition and its cascade of health consequences.
Safety concerns: Inability to detect smoke, gas leaks, or spoiled food creates real dangers. People with anosmia (complete smell loss) face higher accident and injury rates.
Social and emotional effects: Smell plays subtle but important roles in social bonding, mate selection, and emotional regulation. Smell loss correlates with depression, social isolation, and reduced quality of life—factors that themselves predict a shorter lifespan. Diminished sense of smell can also lead to neglect of personal hygiene, increasing safety risks, and impacting overall health.
Cognitive decline: The close neural connections between the olfactory system and memory centers mean that smell loss often tracks with or predicts cognitive problems. A systematic review of 54 studies found strong correlations between smell ability and multiple aspects of cognition.
Smell Loss by Age and Health Status
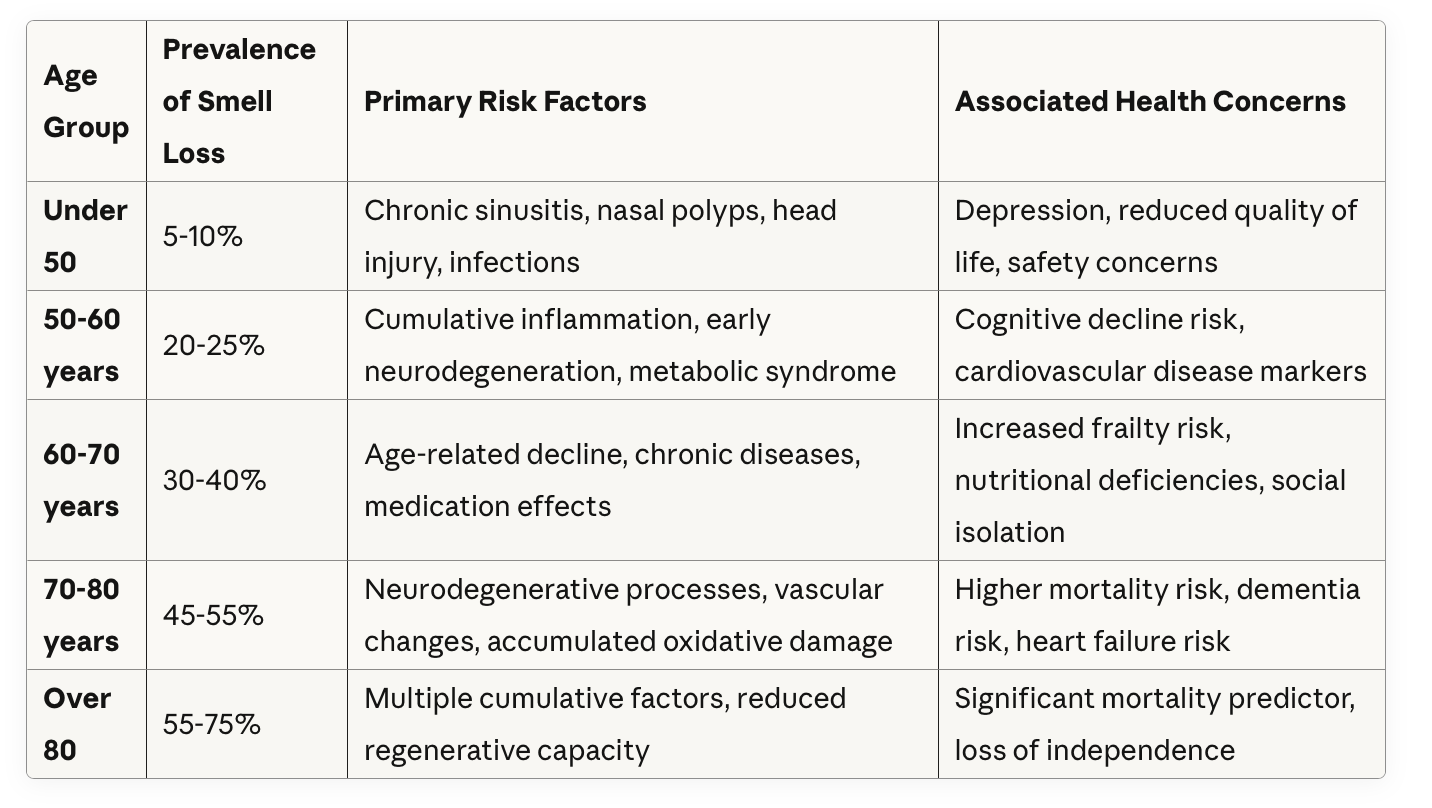
Data compiled from multiple population studies including the National Social Life, Health and Aging Project and published research on olfactory dysfunction prevalence
This chart illustrates why smell testing gains importance with age—it’s precisely when prevalence rises that the mortality prediction becomes most relevant. Older age is associated with increased risk of olfactory dysfunction and related adverse health outcomes. The good news? Interventions to protect smell may also protect overall health.
Protecting Your Sense of Smell—And Your Longevity
Given the powerful connection between sense of smell and longevity, protecting your olfactory function should be a health priority. The ability to detect odors is a key component of olfactory testing and can help identify early changes in smell function. Here are evidence-based strategies:
Get Your Sense of Smell Tested
Simple smell identification tests can establish a baseline and detect early changes. If you notice changes in your ability to smell, discuss testing with your healthcare provider. Early detection allows earlier intervention for underlying conditions and motivation to protect remaining function.
Several validated smell tests exist, including the University of Pennsylvania Smell Identification Test (UPSIT) and shorter screening versions. These tests ask you to identify common odors and compare your score to age-matched norms. By assessing your ability to identify scents, these tests provide important information about your overall health and aging.
Reduce Systemic Inflammation
Since inflammation appears to be the common mechanism linking smell loss to multiple diseases, anti-inflammatory lifestyle strategies protect both your nose and your overall health:
Diet: Follow a Mediterranean-style eating pattern rich in vegetables, fruits, whole grains, legumes, nuts, omega-3 fatty acids from fish, and olive oil. This pattern consistently reduces inflammatory markers and supports brain health.
Exercise: Regular physical activity powerfully reduces systemic inflammation while improving vascular health and supporting neurogenesis (growth of new brain cells, including olfactory neurons).
Sleep: Prioritize 7-8 hours of quality sleep nightly. Sleep deprivation elevates inflammatory markers and impairs the brain's waste clearance system, which may affect olfactory function.
Stress management: Chronic psychological stress drives inflammation through multiple pathways. Find sustainable practices—whether meditation, nature exposure, social connection, or creative activities—that help you manage stress.
Weight management: Excess body fat, particularly visceral fat, produces inflammatory cytokines that affect the entire body, including olfactory neurons.
Try Olfactory Enrichment
Fascinating research from UC Irvine showed that exposing older adults to a variety of pleasant scents for just two hours nightly improved memory performance by 226 percent compared to controls. The mechanism appears to involve reduced inflammation and enhanced neural connectivity.
Lead researcher Michael Leon explains: "Pleasant scents can decrease inflammation, potentially pointing to the mechanism by which such scents can improve brain health."
You don't need expensive devices to try this. Research shows anti-inflammatory effects from common fragrances including:
Essential oils: eucalyptus, lavender, peppermint, limonene (citrus)
Culinary herbs and spices: ginger, oregano, thyme
Natural sources: rose, jasmine, vanilla
Create an olfactory enrichment routine by exposing yourself to different pleasant scents, either through essential oil diffusers, fresh herbs, or natural sources. Vary the scents rather than using the same fragrance repeatedly—diversity appears important for maximal benefit.
Protect Your Nasal Passages
Avoid nasal irritants: Minimize exposure to air pollution, cigarette smoke, harsh chemicals, and other airway irritants that damage olfactory tissue
Manage sinus health: Address chronic sinusitis, allergies, or nasal polyps that physically block odors from reaching olfactory receptors
Consider surgical impacts: Nasal surgery and neck surgery can affect olfactory function. Discuss potential risks with your healthcare provider before undergoing such procedures.
Stay hydrated: Adequate hydration helps maintain the mucus layer that protects olfactory neurons
Be cautious with nasal medications: Some nasal sprays can damage olfactory tissue with prolonged use; follow directions carefully
Support Overall Brain Health
Since the olfactory system connects directly to the brain, strategies that support cognitive health also protect smell:
Maintain social connections: Social isolation accelerates cognitive decline and may affect smell through stress and inflammatory pathways
Challenge your brain: Cognitive engagement through learning, reading, puzzles, or new skills supports neural health throughout the brain, including olfactory pathways
Support your heart health: Manage your blood pressure, blood sugar and cholesterol to keep them in a healthy range
Avoid head injuries: Head trauma can shear neurons at the cribriform plate and damage olfactory neurons, leading to smell loss. Wear appropriate protective equipment during sports and activities
Consider Supportive Nutrition
Certain nutrients support olfactory neuron health and regeneration:
Zinc: Essential for proper smell function; deficiency causes smell loss. Found in oysters, beef, pumpkin seeds, and legumes.
Vitamin A: Supports the epithelial tissues lining the nose. Found in liver, sweet potatoes, carrots, and leafy greens.
Omega-3 fatty acids: Reduce inflammation and support neural membrane health. Found in fatty fish, walnuts, flaxseeds, and chia seeds.
Antioxidants: Vitamins C and E, polyphenols, and carotenoids protect against oxidative damage to olfactory neurons. Found abundantly in colorful vegetables and fruits.
The Future of Smell-Based Health Monitoring
The strong relationship between sense of smell and longevity is opening new frontiers in preventive medicine. Researchers are developing:
Smell tests as screening tools: Simple, inexpensive smell identification tests could become routine health screenings, similar to vision and hearing tests, particularly for older adults. The clinical utility of olfactory testing lies in its ability to improve patient risk stratification and enable early intervention, making it a valuable tool for identifying individuals at high risk of mortality.
Olfactory training programs: Structured exposure to specific scents may help preserve or restore smell function while providing cognitive benefits
Smell-based early detection: Since smell loss often precedes other symptoms, olfactory testing may enable earlier intervention for neurodegenerative diseases
Therapeutic scent delivery devices: Researchers including Dr. Leon are developing devices to deliver controlled olfactory enrichment for brain health
These approaches recognize that the sense of smell isn’t just about enjoying pleasant aromas—it’s a vital health indicator and potential therapeutic target.
The Bottom Line: Your Nose Knows More Than You Think
The connection between sense of smell and longevity represents one of the most intriguing findings in aging research. Your ability to detect and identify odors reflects your inflammatory burden, brain health, and overall physiological resilience. Smell loss isn’t just an inconvenience—it’s a powerful predictor of your longevity that rivals or exceeds many traditional health markers. Olfactory dysfunction can also serve as an early indicator of impending death or critical health decline, enabling earlier intervention to prevent or anticipate severe deterioration.
Rather than accepting smell loss as an inevitable part of aging, we should recognize it as a modifiable risk factor and early-warning system. Protecting your sense of smell through anti-inflammatory lifestyle choices, olfactory enrichment, and proper medical care may protect your brain, your heart, and your longevity.
Pay attention to your nose—it may be trying to tell you something important about your health.
Summary
The olfactory system—anchored by the olfactory bulb and nerve—serves as a vital link between the environment, brain health, and longevity. As research continues to uncover the mechanisms behind olfactory dysfunction and its impact on chronic diseases, smell tests and olfactory testing are poised to become essential tools in predicting mortality and safeguarding the health of older adults. The study suggests that protecting your sense of smell may be one of the most important steps you can take to support your brain, your body, and your future.
Frequently Asked Questions
Is loss of smell normal with aging?
It’s common—affecting ~25% in their early 50s and >50% over 80—but it’s not trivial, as it tracks with broader health risks.
Why does smell loss link to so many conditions?
Evidence points to inflammation as a shared driver. The olfactory system connects directly to the brain, so systemic or neural inflammation may first appear as diminished smell.
Is smell loss a cause or just a marker?
It may be both. Studies suggest smell impairment predicts cognitive decline and mortality; researchers propose at least some causal relationships via inflammation.
Can “smell training” really help?
Early research in older adults shows olfactory enrichment can improve memory performance and may reduce inflammatory responses to pleasant scents.
What scents are practical to start with?
Culinary herbs/spices and essential oils: ginger, oregano, thyme, eucalyptus, lavender, peppermint, citrus (limonene), and even familiar food aromas. Rotate 2 to 4 scents, twice daily, for 12+ weeks.
UC Irvine News: Smell loss linked to 100-plus diseases in new UC Irvine study October 29, 2024
Leon M, et al. Inflammation and olfactory loss are associated with at least 139 medical conditions Front Mol Neurosci. 2024 Oct 11;17:1455418
Woo, C.C., et al. (2023). “Overnight olfactory enrichment using an odorant diffuser improves cognition in healthy older adults.” Frontiers in Neuroscience, 17:1200448.
Ruane, R., et al. (2025). “Olfactory Deficits and Mortality in Older Adults.” JAMA Otolaryngology–Head & Neck Surgery.
Yeo, B.S.Y., et al. (2024). “Olfactory Impairment and Frailty: A Systematic Review and Meta-analysis.” JAMA Otolaryngology–Head & Neck Surgery.
Zhou, C., et al. (2024). “Valid olfactory impairment tests can help identify mild cognitive impairment: A meta-analysis.” Frontiers in Aging Neuroscience, 16:1349196.
Stem Cell Restore
Increased Energy from Organic Tibetan Sea Buckthorn Trans-Resveratrol, Vitamin D



