You’ve been told for years that your HDL cholesterol—the “good” kind—is a badge of health. But what if that same number your doctor celebrates is silently sabotaging your memory? New research reveals a startling truth that could reshape how women navigate brain health during menopause—and it’s not about how much HDL you have, but how well it’s actually working.
Key Takeaways
- HDL Quality is Better Than Quantity: Large HDL particles, once thought to be protective, may increase memory loss risk in menopausal women.
- Menopause Reshapes Cholesterol Function: Hormonal shifts can transform “good” HDL into dysfunctional particles that promote inflammation and arterial damage.
- Advanced Testing is Crucial: Standard cholesterol panels miss key markers. Testing for HDL particle size, hormone levels, and inflammation offers a clearer picture of brain and heart risk.
The "Good" Cholesterol Myth That's Been Hurting Women
Picture this: You’re 52, going through menopause, and you’ve been diligently following your doctor’s advice to keep your HDL cholesterol above 60 mg/dL. You’ve been told this “good” cholesterol will protect your heart and brain from aging. But lately, you’re struggling to remember names, losing your keys regularly, and feeling like your brain is wrapped in cotton. You mention this to your doctor, who dismisses it as “normal menopause” and congratulates you on your excellent HDL levels. However, menopause symptoms can sometimes mimic or overlap with more serious health conditions, such as cardiovascular disease, making it crucial to understand these symptoms and the associated risk factors that impact women's health.
Here’s what’s shocking: that high HDL might actually be contributing to your memory problems.
For decades, the medical establishment has pushed the narrative that higher HDL cholesterol equals better health. We’ve been told it acts like a biological vacuum cleaner, sucking up dangerous LDL cholesterol and protecting our arteries and brains. But emerging research from top medical institutions is turning this conventional wisdom on its head, especially for women navigating menopause. It’s increasingly important to consider risk factors beyond just cholesterol numbers, particularly during menopause, when hormonal changes and lifestyle factors can significantly affect cardiovascular health.
Size Matters More Than Numbers
Dr. Samar El Khoudary and her team at the University of Pittsburgh School of Public Health have been quietly revolutionizing our understanding of cholesterol and brain health. Their focus? How HDL affects postmenopausal women, a group that’s been largely overlooked in cardiovascular and cognitive research.
What they discovered is nothing short of revolutionary: it’s not the amount of HDL cholesterol that matters for brain health, it’s the size and functionality of the HDL particles themselves.
Think of HDL particles like delivery trucks carrying cholesterol. Some are large trucks, some are medium-sized, and others are small and nimble. For years, we’ve been counting the number of trucks without paying attention to whether they’re actually doing their job effectively.
The stunning finding: large HDL particles in menopausal women don’t just fail to protect the brain, they may actually harm it. These changes in HDL particle size also have important implications for cardiovascular risk in postmenopausal women, highlighting the need to assess and manage this risk to reduce the likelihood of heart attack and stroke.
Why Menopause Changes Everything for Women
Menopause isn’t just about hot flashes and mood swings. It’s a complete biological revolution that affects every system in your body, including how your cholesterol functions and how your body manages lipid metabolism.
The Hormonal Hurricane
When estrogen levels plummet during menopause, it triggers a cascade of changes that affect cholesterol metabolism, brain function, and vascular health. Estrogen isn’t just a reproductive hormone, it’s a powerful neuroprotective agent that:
- Acts as a neurosteroid, promoting brain plasticity and memory formation
- Protects blood vessels from inflammation and damage
- Helps regulate cholesterol particle size and function
- Maintains the integrity of the blood-brain barrier
- Plays a crucial role in regulating lipid metabolism and maintaining healthy cholesterol levels
As estrogen levels decrease during the menopause transition, these protective effects are lost, which can impact cholesterol and cardiovascular health by increasing LDL and triglycerides and raising the risk of heart disease.
As estrogen disappears, the protective systems it supported begin to break down, leaving women vulnerable to cognitive decline and cardiovascular disease.
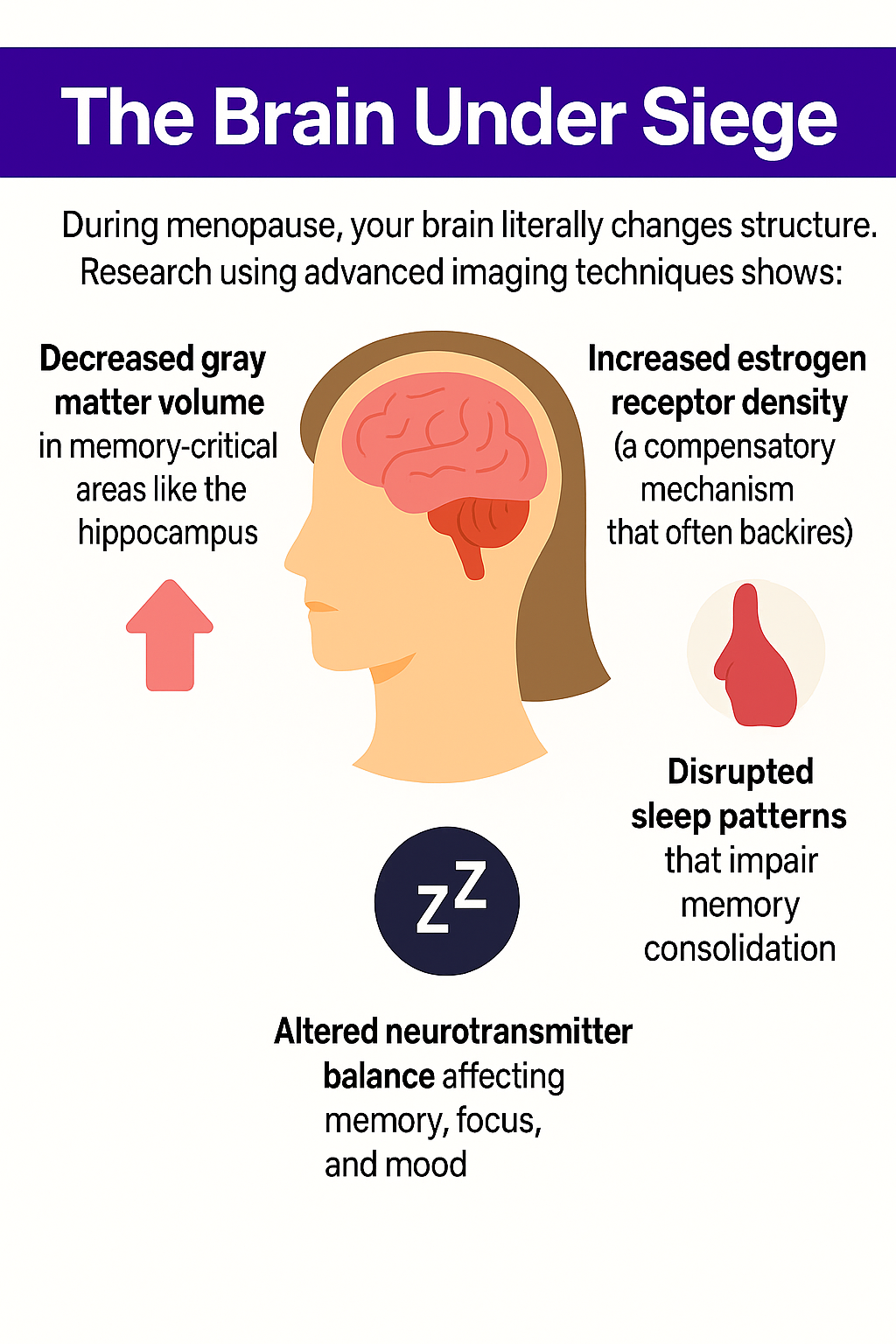
This biological upheaval creates the perfect storm for the memory issues that plague so many menopausal women. These are issues that doctors too often dismiss as “just part of getting older.” Changes in lipid metabolism during the menopause transition can also impact cholesterol levels, further increasing the risk for cardiovascular and cognitive health problems.
The Pittsburgh Studies That Changed Everything
Study #1: The Arterial Wake-Up Call (2018)
Dr. El Khoudary’s first bombshell came in 2018 when her team studied 1,138 women aged 45-84. They discovered something that shocked the medical community: higher HDL cholesterol levels were linked to higher levels of arterial plaque.
“Higher HDL cholesterol may not always be as protective in postmenopausal women as we once thought,” Dr. El Khoudary commented, a statement that sent ripples through the medical establishment.
It’s important to note that low-density lipoprotein (LDL), often called 'bad cholesterol', is typically associated with increased cardiovascular risk because it transports cholesterol to the arteries, contributing to plaque buildup. The interplay between HDL and LDL is complex, especially during menopause.
However, the real revelation came when they examined the particle sizes. Women with high numbers of large HDL particles had an increased risk of heart disease near menopause, while those with more small HDL particles showed a lower risk.
Study #2: The Dysfunction Discovery (2022)
The follow-up study was even more damning. Large HDL particles not only become less protective during menopause, but they also become actively harmful, promoting arterial calcification and inflammation.
It was like discovering that your security guards had joined the enemy team.
Study #3: The Memory Connection (2024)
The latest study, published in The Journal of Clinical Endocrinology and Metabolism, followed over 500 women for 16 years, tracking both their cholesterol particles and cognitive function.
The results were stark:
Women with larger HDL particles had worse memories and poorer cognitive performance
Women with smaller HDL particles rich in phospholipids had better immediate recall, delayed recall, and faster processing speed
The dysfunction of large particles correlated directly with memory decline
This wasn't just correlation, t was a clear biological pathway showing how certain types of "good" cholesterol were actually harming women's brains.
The High HDL Danger Zone and Cardiovascular Disease Risk Factors
Here’s what’s particularly concerning: current medical guidelines recommend HDL levels above 60 mg/dL for optimal health. But recent studies suggest that levels above 65 mg/dL may actually increase dementia risk by 15%.
This means millions of women with “excellent” cholesterol numbers might unknowingly be at higher risk for cognitive decline. Women who are considered high risk—due to other risk factors such as family history, menopause, or pregnancy-related conditions—may need a more comprehensive assessment that takes into account their lifetime risk for cardiovascular events and cognitive decline.
One woman shared her experience: “My doctor was thrilled with my HDL of 78 mg/dL. She said I had the cholesterol profile of a marathon runner. But I couldn’t remember conversations from the day before, and I was making mistakes at work that I’d never made in 20 years of practice.”
The Science Behind the Dysfunction
Why Large HDL Particles Go Rogue
During menopause, large HDL particles undergo structural changes that impair their function:
Loss of Anti-Inflammatory Properties: Instead of reducing inflammation, dysfunctional large HDL particles can promote it
Impaired Cholesterol Transport: They become less efficient at removing cholesterol from arterial walls
Oxidative Stress: Large particles become more susceptible to oxidation, turning them from protectors into promoters of vascular damage
Blood-Brain Barrier Disruption: Dysfunctional HDL may contribute to increased permeability of the blood-brain barrier, allowing inflammatory substances to reach the brain
The Small Particle Advantage
Small, dense HDL particles rich in phospholipids maintain their protective properties during menopause:
-
Enhanced Anti-Inflammatory Activity: They continue to reduce systemic inflammation
Better Antioxidant Function: More resistant to oxidative damage
Improved Brain Protection: Better able to support blood-brain barrier integrity
Efficient Cholesterol Removal: Maintain their "vacuum cleaner" function for arterial health
Beyond Numbers: What Your Doctor Should Be Testing
Standard cholesterol panels only tell part of the story. Dr. El Khoudary and other specialists believe doctors need to look beyond basic lipid numbers to include:
Advanced testing such as lipid metabolomics, which provides a more detailed analysis of blood cholesterol levels and their impact on health.
Hormone levels, especially estrogen and progesterone, are used to understand how hormonal changes affect lipid profiles and cardiovascular risk.
Inflammatory markers, which can indicate underlying risk for heart disease and cognitive decline.
Family history, as having a family history of high cholesterol or cardiovascular disease, significantly increases risk and should be considered when assessing cardiovascular and cognitive risk.
Advanced Cholesterol Testing
- Total cholesterol
- HDL particle size and number
- HDL composition (especially phospholipid content)
- HDL functionality tests
- Inflammatory markers like hsCRP
- Apolipoprotein A-I levels
Comprehensive Hormone Assessment
- Estradiol levels
- Testosterone(often overlooked but important for brain health)
- Thyroid function
- Cortisol patterns
Cognitive Screening
- Memory and attention tests
- Processing speed assessments
- Executive function evaluation
These tests are available but often require seeking out specialists familiar with advanced lipid analysis and menopausal medicine.
The Menopausal Woman's Memory-Protecting Action Plan
Step 1: Optimize HDL Quality, Not Just Quantity
Focus on interventions that improve HDL function rather than just raising HDL levels:
Exercise That Matters:
- Aerobic exercise increases small, protective HDL particles
- Resistance training improves HDL functionality
- High-intensity interval training (HIIT) can boost both particle quality and brain-derived neurotrophic factor (BDNF)
Strategic Nutrition:
- Mediterranean diet rich in olive oil, nuts, and fatty fish
- Include monounsaturated fats and healthy fats such as olive oil, avocados, and nuts to support heart and brain health
- Limit saturated fats from sources like red meat, high-fat dairy, and processed meats to lower LDL cholesterol
- Increase soluble fiber intake from foods like oats, beans, and fruits to help lower cholesterol
- Incorporate soy protein, soy milk, and soy nuts as plant-based protein sources that can help lower LDL cholesterol and support hormonal balance
- Emphasize dietary strategies to lower LDL cholesterol, which are especially important during menopause
- Omega-3 fatty acids from fish or high-quality supplements
- Antioxidant-rich foods like berries, dark leafy greens, and colorful vegetables
- Limit processed foods and refined sugars that promote HDL dysfunction
Step 2: Address Hormonal Imbalances
Consider Hormone Replacement Therapy (HRT)
The “critical window” hypothesis suggests that estrogen therapy started early in menopause (within 5 years) may:
- Preserve HDL functionality
- Protect against cognitive decline
- Maintain vascular health
- Support brain structure and function
Women who experience early menopause (before age 45) may have different cardiovascular and cognitive risks, so it is especially important for them to discuss hormone therapy options and risk assessment with their provider. Post-menopause, hormonal changes can continue to impact cognitive and cardiovascular health, making ongoing assessment and management important.
However, HRT isn’t right for everyone and requires careful discussion with a knowledgeable provider about individual risks and benefits.
Natural Hormone Support:
- Phytoestrogens from soy, flax seeds, and red clover
- Adaptogenic herbs like ashwagandha for cortisol balance
- Sleep optimization to support natural hormone production
Step 3: Implement Brain-Protective Lifestyle Strategies
Sleep Optimization:
- Address night sweats and insomnia, which disrupt memory consolidation and sleep quality
- Maintain consistent sleep schedules
- Create a cool, dark sleep environment
- Consider cognitive behavioral therapy for insomnia (CBT-I)
Stress Management:
- Chronic stress elevates cortisol, which impairs HDL function and memory
- Mindfulness meditation can reduce cortisol and improve cognitive function
- Regular yoga practice supports both stress reduction and brain health
- Deep breathing exercises activate the parasympathetic nervous system
- Managing mood changes that accompany menopause can help alleviate symptoms and support emotional well-being
Cognitive Training:
- Engage in novel learning activities that challenge the brain
- Learn new languages, musical instruments, or complex skills
- Social engagement and meaningful relationships
- Limit multitasking, which can overwhelm the menopausal brain
Step 4: Target Inflammation
Since dysfunctional HDL promotes inflammation, focus on anti-inflammatory strategies. Chronic inflammation increases cardiovascular disease risk and can damage the cardiovascular system, raising the likelihood of heart attack or stroke.
Supplement Considerations:
- Curcumin
- High-quality fish oil with EPA and DHA
- Resveratrol for vascular protection
- Magnesium for sleep and stress support
Inflammatory Food Elimination:
- Reduce or eliminate ultra-processed foods
- Limit added sugars and refined carbohydrates
- Identify and address food sensitivities
- Consider an elimination diet to identify triggers
Real Women, Real Results
"After learning about HDL particle size, I asked my doctor for advanced testing. My HDL was 72 mg/dL—supposedly excellent—but I had mostly large, dysfunctional particles. We focused on improving particle quality through diet and exercise rather than just raising HDL numbers. Within six months, my brain fog lifted, and my memory sharpened dramatically." – Sarah, 54
"I was told my high HDL meant I didn't need to worry about heart or brain health. But I was struggling with words, forgetting appointments, and feeling mentally sluggish. When I switched to a Mediterranean diet and started strength training, not only did my memory improve, but follow-up testing showed my HDL particles had shifted from large to small and functional." – Maria, 49
The Future of Cholesterol Testing
Since cholesterol chemistry is complex, Dr. El Khoudary and other specialists think doctors need to look beyond standard lipid panels to include the size, shape, and composition of cholesterol particles. Such tests are available, but harder to get through standard clinician visits
The paradigm shift toward measuring cholesterol quality rather than just quantity represents a revolution in preventive medicine. Advanced testing that evaluates:
Particle size distribution
Inflammatory status
Oxidative stress markers
This comprehensive approach provides a much clearer picture of cardiovascular and cognitive risk than traditional panels.
The Takeaway: Redefining "Good" Cholesterol
The revelation that HDL quality matters more than quantity represents a seismic shift in how we approach cholesterol and brain health during menopause. For too long, women have been told that high HDL numbers guarantee protection, while their very real cognitive symptoms were dismissed.
This research validates what many women have been experiencing: despite "perfect" cholesterol numbers, they're still struggling with memory, focus, and mental clarity. The problem isn't with them—it's with our understanding of how cholesterol functions in the menopausal brain.
The new paradigm focuses on:
HDL particle quality over quantity
Comprehensive hormone optimization
Anti-inflammatory lifestyle strategies
Advanced testing that reveals the full picture
Validation of women's cognitive concerns
As Dr. El Khoudary noted optimistically: "Even though higher levels of HDL cholesterol may not be protective as you get older, there are things you can do that might help improve the quality of HDL particles, even as early as your 40s."
Try Life’s Essential Eight
Dr. El Khoudary recommends following Life’s Essential 8, an updated version of Life’s Simple Seven. This involves addressing four key health behaviors and four key health factors. These are:
· Eat better
· Be more active
· Quit tobacco
· Get healthy sleep
· Manage weight
· Control cholesterol
· Manage blood sugar
· Manage blood pressure
Midlife women should prioritize these essential health behaviors to reduce their risk of chronic diseases. While some women may be at low risk for cardiovascular disease, others may require more intensive interventions based on their individual health profiles. Breast cancer is often a major health concern for women, but it is important not to overlook the significant risk of cardiovascular disease during menopause and midlife.
The message is clear: don’t let anyone dismiss your brain fog as “just menopause.” Armed with this new understanding, you can advocate for proper testing, appropriate treatment, and the cognitive support you deserve. Your brain—and your future self—will thank you for taking this seriously.
Summary
New research upends long-standing beliefs about HDL cholesterol in women, especially during menopause. While high HDL levels have traditionally been viewed as protective for heart and brain health, recent studies show that large HDL particles may actually harm memory in postmenopausal women. The functionality and size of HDL particles—not just their quantity—play a critical role in cognitive and cardiovascular outcomes. Addressing hormone balance, inflammation, and particle quality may offer new hope for women battling brain fog and memory decline.
Frequently Asked Questions
If my HDL is high, should I be worried?
Not necessarily, but Dr. El Khoudary considers it one of the heart disease risk factors so it's worth investigating. High HDL with good particle quality and function can still be protective. The key is advanced testing to determine particle size and functionality.
Can I improve my HDL particle quality naturally?
Yes! Exercise, Mediterranean diet, omega-3 fatty acids, and stress management can all improve HDL functionality. Some women also benefit from hormone therapy under medical supervision.
How long does it take to see improvements in brain fog and memory?
Many women notice improvements in 2-4 weeks with exercise and dietary changes. Hormone therapy, when appropriate, often shows benefits within 1-3 months. Consistency is key.
Is this just about menopause, or do younger women need to worry too?
This research specifically applies to menopausal women due to hormonal changes. However, the principles of focusing on HDL quality over quantity likely benefit women of all ages.
1 University of Pittsburgh ‘Good Cholesterol’ May Not Always be Good for Postmenopausal Women 7/19/2018
2 Clinical Advisor, “HDL Is Not Always Good Cholesterol During Menopause Transition,” October 17, 2022
3 University of Pittsburgh HDL quality, not quantity, contribute to the first sign of Alzheimer’s disease in women October 11, 2024
My Heart Miracle
Scientifically proven to help increase energy at the cellular level while actually boosting the cholesterol-fighting effects of your medication


